A food intolerance test is often the first thing people search for when bloating becomes frequent, unpredictable, and frustrating, especially when it seems to happen “no matter what I eat.” The truth is that bloating is rarely caused by one single food. More often, it’s a pattern shaped by digestion, gut sensitivity, hormones, stress, sleep, hydration, and what you’re eating around your triggers.
At Siam Clinic, we see this often in travelers who arrive feeling great, then suddenly develop bloating in a tropical routine. A change in meal timing, spicy foods, alcohol, heat-driven dehydration, and long-haul flights can all shift digestion. The goal is not to fear food, but to identify what your body struggles to process, and do it in a medically sound way.
Bloating is a symptom, not a diagnosis
Bloating can feel like “gas,” “water retention,” or pressure that builds throughout the day. Common drivers include:
- Carbohydrate fermentation (certain fibers and sugars create more gas)
- Constipation or slow gut transit
- Irritable bowel syndrome (IBS) and visceral hypersensitivity
- Lactose intolerance or other malabsorption issues
- High-FODMAP foods (fermentable carbohydrates)
- Stress, poor sleep, and meal speed (swallowed air and gut-brain signaling)
- Hormonal fluctuations (often cyclical)
- Carbonated drinks, sugar alcohols, and large late meals
A “food intolerance” can be part of the picture, but testing needs to be chosen carefully. Some popular panels are not clinically meaningful and may lead to unnecessary restriction.
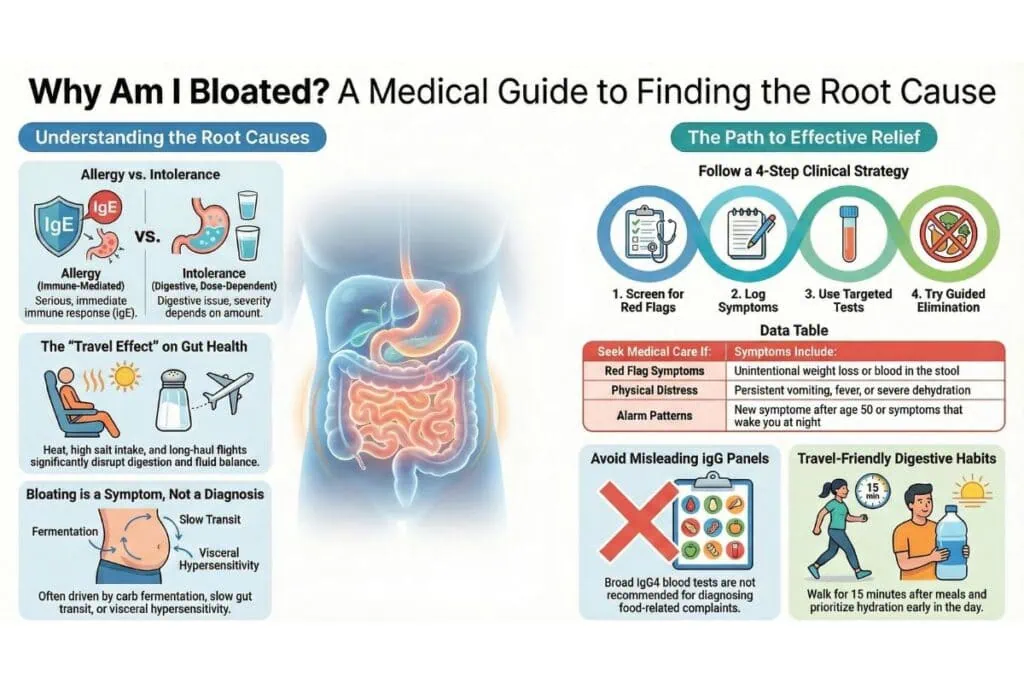
Food allergy vs food intolerance: why the difference matters
People often use “allergy” and “intolerance” interchangeably, but medically they are different.
Food allergy (immune-mediated, can be serious)
- Often involves IgE mechanisms
- May cause hives, swelling, wheeze, throat tightness, vomiting, or severe reactions
- Should be evaluated promptly, especially with any red-flag symptoms
Food intolerance (digestion or sensitivity related)
- Not typically IgE-mediated
- More commonly causes bloating, gas, cramps, diarrhea, or fatigue
- Often dose-dependent (small amount may be tolerated, large amount may trigger symptoms)
If symptoms include breathing difficulty, facial swelling, fainting, or rapid-onset widespread hives, do not self-test. Seek urgent medical care.
What a “food intolerance test” can realistically tell you
There isn’t one perfect, universal test that “finds all intolerances.” The most useful approach depends on your symptoms and medical history. In practice, a good work-up often combines targeted testing plus a structured elimination and reintroduction plan.
Helpful, evidence-supported testing options
1) Lactose intolerance testing
Lactose intolerance is one of the most common reasons for dairy-related bloating. Testing may include breath testing or supervised dietary trials, depending on local availability and clinical judgment.
2) Celiac disease screening (when appropriate)
Celiac disease is not an intolerance. It is an immune-mediated condition triggered by gluten that can cause bloating, diarrhea, anemia, fatigue, and nutrient deficiencies. If suspected, screening blood tests may be considered before removing gluten, because going gluten-free first can affect accuracy.
3) Breath testing for specific malabsorption or overgrowth patterns (selected cases)
In some people with persistent bloating, clinicians may consider breath testing to assess patterns consistent with carbohydrate malabsorption or small intestinal bacterial overgrowth. Results require careful interpretation because false positives and false negatives can occur.
4) Stool tests (in selected cases)
Sometimes used to evaluate inflammation markers or infection risk when symptoms suggest more than functional bloating.
Tests that are commonly misunderstood: IgG “food sensitivity” panels
Many commercial blood panels claim to diagnose “food intolerance” by measuring IgG or IgG4 antibodies to dozens of foods. In clinical immunology, food-specific IgG often reflects exposure and immune recognition, not intolerance. A well-cited position paper concludes IgG4 testing for foods is not recommended for diagnosing food-related complaints.
A result that labels many foods as “positive” can lead to overly restrictive diets, stress around eating, and nutritional imbalance, without actually addressing the root cause.
Why bloating can worsen when you travel
Even when meals look “healthy,” travel changes physiology:
- Heat and humidity can increase fluid shifts and dehydration risk
- More salt from restaurant meals can increase water retention and abdominal distension
- Alcohol plus sun exposure can disrupt sleep and gut motility
- Long flights reduce movement and slow digestion
- New spices and higher fat meals can change gastric emptying
- Stress and schedule changes affect the gut-brain axis
Many visitors in Phuket notice bloating builds throughout the day, especially when meals are late and hydration is inconsistent. This is why a testing plan should include lifestyle context, not just a lab result.
Food intolerance test strategy that clinicians prefer
When bloating is the primary issue, a practical clinician-led strategy usually follows this order:
Step 1: Screen for red flags
Seek medical evaluation if you have:
- Unintentional weight loss
- Blood in stool or black stool
- Persistent vomiting
- Fever, severe diarrhea, or dehydration
- New symptoms after age 50
- Strong family history of gastrointestinal cancer or inflammatory bowel disease
- Night-time symptoms that wake you regularly
Step 2: Identify patterns (before testing)
A 7 to 14-day symptom log is often more valuable than guessing:
- Time of meals
- Bloating severity (0–10)
- Stool pattern
- Sleep
- Stress level
- Alcohol and caffeine
- Key foods (dairy, wheat, onions, garlic, legumes, carbonated drinks)
Step 3: Use targeted tests, not broad panels
The goal is to test what is plausible:
- Dairy-trigger pattern: consider lactose strategy
- Gluten-related systemic symptoms: consider celiac screening discussion
- IBS-like pattern: consider dietary approach first, testing selectively
Step 4: Do a structured elimination and reintroduction
This is where many people go wrong by cutting everything at once.
A clinician-guided plan may include:
- Remove one category (for example lactose) for 10–14 days
- Reintroduce with a clear dose challenge
- Observe symptoms and repeat with the next category if needed
For IBS-type symptoms, a short-term low-FODMAP trial may help reduce bloating in some people, then foods are reintroduced to find personal thresholds. Clinical guidance is helpful because long-term restriction is not the goal.
If it’s not intolerance, what else could it be?
Bloating is often functional, meaning the gut is structurally normal but reacts strongly to certain stimuli. Common scenarios:
Functional bloating and IBS patterns
- Bloating worsens after meals
- Symptoms fluctuate with stress and sleep
- Alternating constipation and diarrhea may occur
- Certain fermentable foods trigger symptoms more than “calories” do
Constipation-driven bloating
If stool transit is slow, gas and pressure build. This can happen even if you have daily bowel movements, especially if evacuation is incomplete.
Swallowed air and rapid eating
Eating quickly, chewing gum, carbonated drinks, and talking while eating can increase swallowed air.
Hormonal and fluid shifts
Some people experience cyclical bloating linked to hormonal changes. Salt intake, hydration, and sleep can amplify it.
Travel-friendly tips to reduce bloating without over-restricting
If you’re visiting Phuket, these simple steps can support digestion while you explore:
- Hydrate early, not only at night
- Choose one “lighter meal” daily (protein + cooked vegetables is often easier)
- Walk 10–15 minutes after meals
- Limit carbonated drinks, especially with large dinners
- Keep alcohol to smaller amounts, and avoid mixing alcohol with very salty meals
- Use a consistent breakfast routine for 3–4 days to stabilize digestion
- If dairy is a suspected trigger, choose lactose-free options temporarily rather than cutting all nutrition groups
Results vary by individual, but these habits can reduce symptom intensity while you work on the root cause.
FAQ
1) Is a food intolerance test accurate for bloating?
Some targeted tests can be useful, depending on your symptoms. Broad IgG “food sensitivity” panels are not considered reliable for diagnosing intolerance and may lead to unnecessary restrictions.
2) How long does it take to see improvement after removing a trigger food?
Many people notice changes within 7–14 days, but patterns like constipation-driven bloating or IBS-type sensitivity may take longer and often need a combined approach.
3) Can stress cause bloating even if my diet is clean?
Yes. Stress can change gut motility, sensitivity, and the gut-brain signaling that influences bloating, especially during travel or disrupted sleep.
4) Should I cut gluten if I feel bloated?
Not automatically. If celiac disease is a concern, it’s better to discuss screening before removing gluten, because eliminating gluten early can affect test interpretation.
5) What are warning signs that mean I should stop self-treating and see a doctor?
Weight loss, blood in stool, severe persistent diarrhea, fever, ongoing vomiting, dehydration, or symptoms that wake you at night should be evaluated promptly.
Recommended Next Reads
- Comparison Between Hangover IV Drip and Dehydration Therapy
- Liver Detoxification Explained What Works and What Doesn’t
- IV Drip Therapy in Phuket Why Everyone Is Talking About It
Sources
- PubMed: Testing for IgG4 against foods is not recommended as a diagnostic tool
- NIH (NIDDK): Irritable Bowel Syndrome overview
If you’re visiting Phuket and would like personalized wellness guidance during your stay, Siam Clinic is here to help you choose a sensible testing pathway, interpret results safely, and build a plan that fits real life, not restrictive rules.